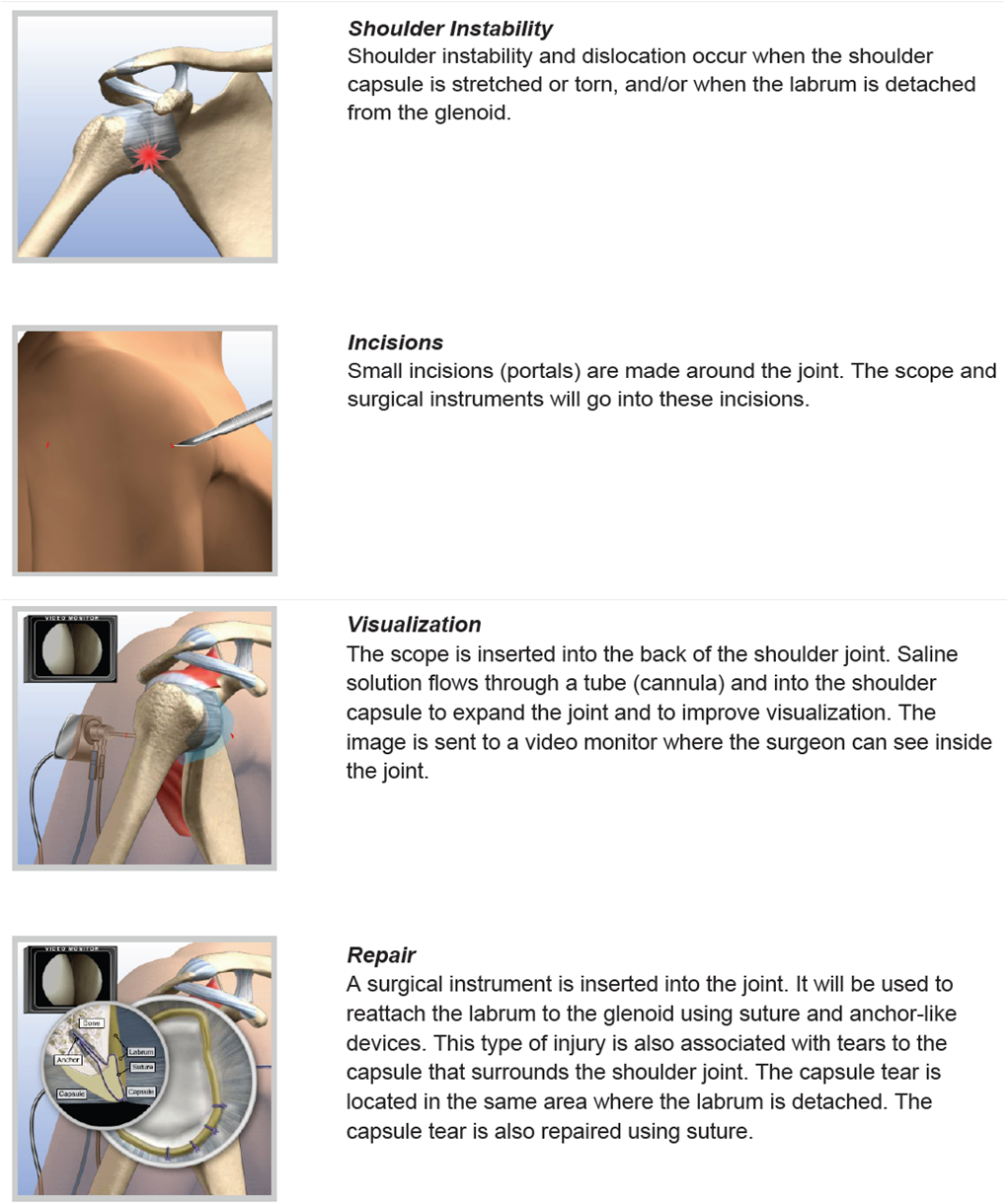
Shoulder Instability
The shoulder has the largest range of movement of any joint in the body. The ability to move the arm in all directions comes at the expense of stability. Instability occurs when the ball is forced out of its shallow socket as a result of sudden injury or due to a loose joint. Once it has dislocated it is vulnerable to recurrent episodes.
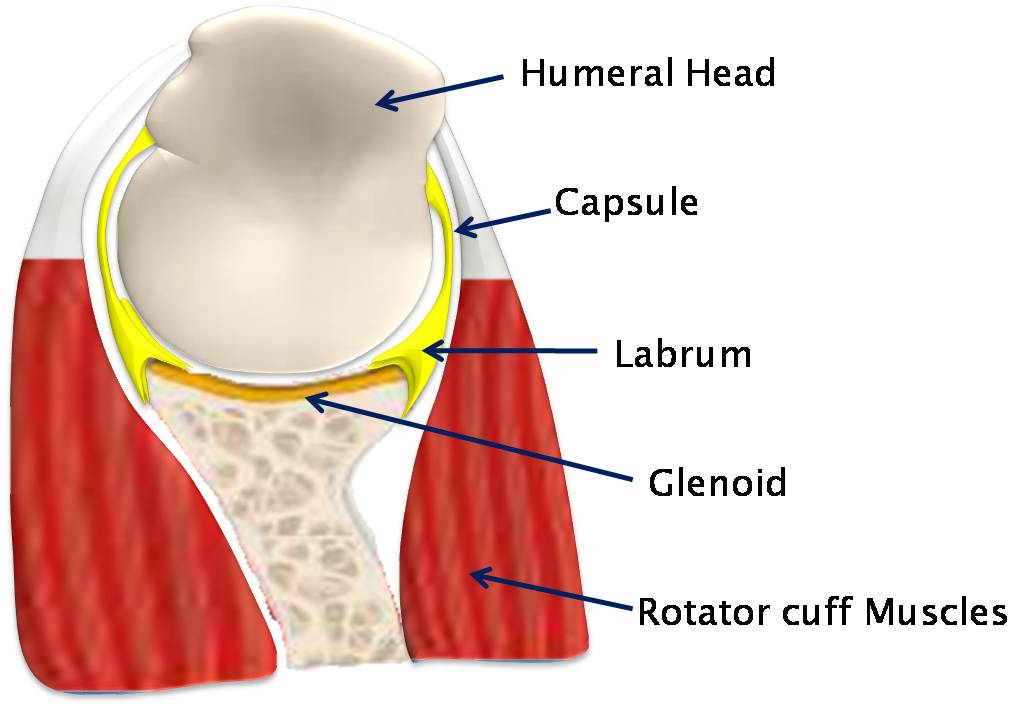
Normal shoulder anatomy
Your shoulder is made up of three bones: your upper arm bone (humerus), your shoulder blade (scapula), and your collarbone (clavicle).
The head, or ball, of your upper arm bone fits into a shallow socket (glenoid) in your shoulder blade. It is like a golf ball sitting on a golf tee and liable to fall off. To help prevent this; strong connective tissues form a ligament system (labrum and capsule) which keeps the head of the upper arm bone centered in the glenoid socket. Shoulder stability also relies on contraction of the strong tendons and muscles which surround the head and socket (rotator cuff).
There are three main types of instability
1) Traumatic structural.
This is the commonest type and occurs when the shoulder is forced out of its socket due to a fall or a direct impact. This often occurs as a result of injury during a rugby match, surfing or falling off a horse. The force is so great that it tears the labrum and ligaments off the socket (Bankart tear). Without these check rains the joint becomes unstable and repeated dislocations are common.
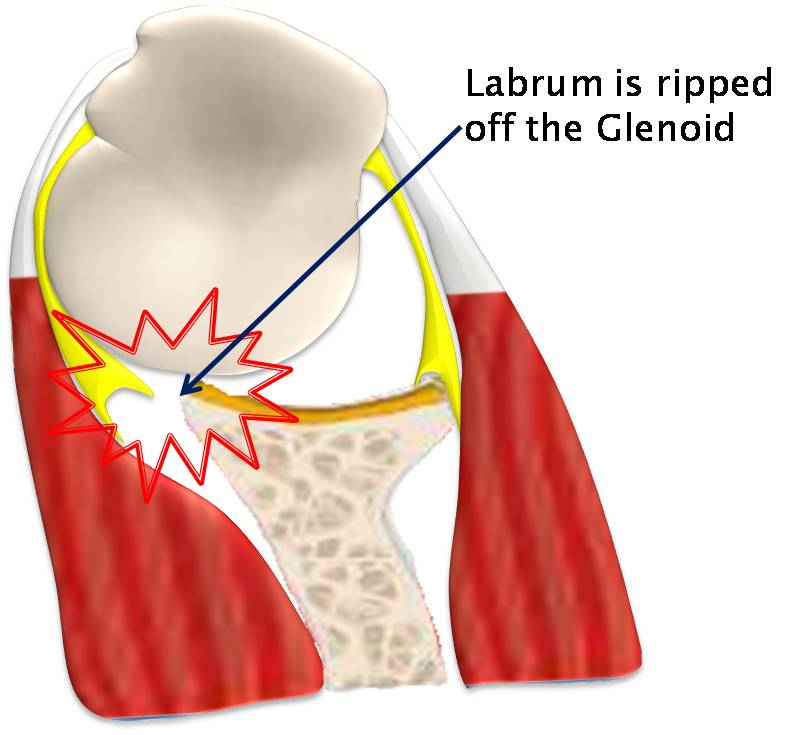
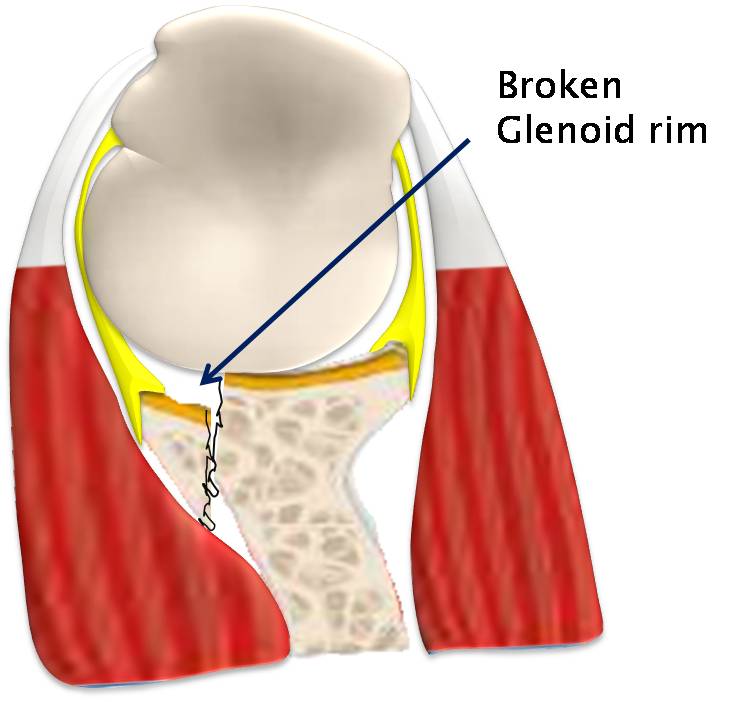
Bony Bankart: When the head is driven out it can knock off the bony edge of the glenoid. This results in gross instability and recurrent dislocations are inevitable.
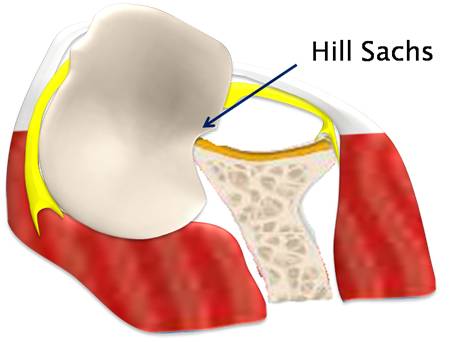
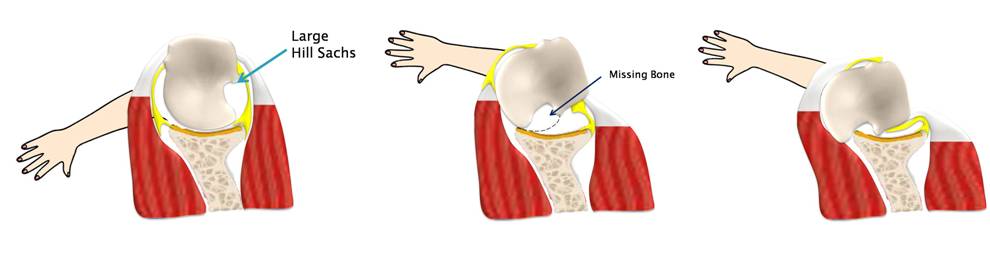
Hill Sachs: a dent in the back of the humeral head which occurs during the dislocation as the humeral head impacts against the front of the glenoid.
Engaging Hill sachs: If the dent occurs on the joint surface of the humeral head, it will engage with the glenoid as the arm is rotated. The missing bone will allow it to fall of the glenoid.
2) Atraumatic dislocation.
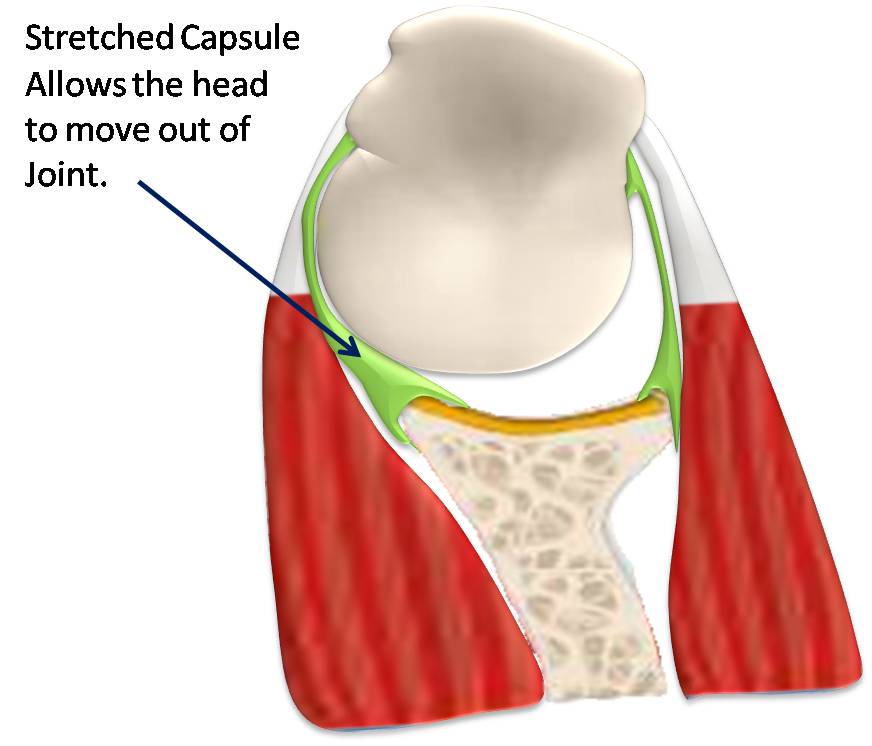
This occurs when the shoulder is loose and dislocates with only a small force such as reaching out for an object or when turning in bed. It will often clunk back in without the need to go to casualty. This type of dislocation occurs in 'lax' joints, for example people who are able to bend their knees and elbows the wrong way. This joint laxity usually remains trouble free, however if the muscles around the shoulder start to pull in one direction more than the other; it is enough for a lax joint to become unstable. Other patients have a repetitive strain to the capsule which lengthens it. The capsule in the shoulder becomes stretched, so the check rains are less precise in centralising the head in the glenoid socket. Referral for appropriate physiotherapy is the initial form of management. The physiotherapist should look at the way in which the muscles and shoulder joint is moving and posture aiming to restore the balance. Treatment can 'cure' the problem as long as the exercises and advice is continued, but in some cases there is only minimal benefit. For these patients surgical intervention is indicated.
3) Muscle patterning
Muscle Patterning refers to inappropriate recruitment of the muscles of the shoulder joint e.g. Latissimus Dorsi, Pectoralis Major, Anterior/Posterior Deltoid, resulting in uncontrolled translation of the humeral head and often subluxation or dislocation of the joint. This unbalanced muscle action is involuntary and ingrained. Patients with muscle patterning essentially have a muscle recruitment sequencing problem that results in abnormal force couples destabilising the joint.
How do I know if I have shoulder instability?
Common symptoms of chronic shoulder instability include:
Pain caused by shoulder injury
Repeated shoulder dislocations
Repeated instances of the shoulder giving out
A persistent sensation of the shoulder feeling loose, slipping in and out of the joint, or just "hanging there"
What is the non surgical Treatment?
It often takes several months of nonsurgical treatment before you can tell how well it is working. Nonsurgical treatment typically includes:
Activity modification. You must make some changes in your lifestyle and avoid activities that aggravate your symptoms.
Non-steroidal anti-inflammatory medication. Drugs like aspirin and ibuprofen reduce pain and swelling.
Physical therapy. Strengthening shoulder muscles and working on shoulder control can increase stability. Your therapist will design a home exercise program for your shoulder.
What is the Surgical Treatment?
What should I expect during recovery?
Once the numbness has worn off (4-8 hours) the shoulder will become painful after the operation if you do not take regular pain killers as soon as you get home. Even though you may be pain free at rest you must take the tablets for when you move the shoulder as part of your rehabilitation program. A combination of regular painkillers such as paracetamol or codeine should be taken with NSAIDs (unless contra-indicated) such as ibuprofen- which is also an anti inflammatory drug. If the pain killers you have been given are not sufficient please contact your consultant's secretary or your GP. The little incisions are covered with a small sticky dressing which should be kept dry and replaced with spare dressings when necessary. You will be given these before leaving hospital. You will be given a sling which will protect your shoulder and help with pain relief.
You will need a dedicated physiotherapy program after your surgery. If you have been seeing a physiotherapist prior to your surgery (who may have referred you to Guildford Upper Limb), you should arrange to see them afterwards so you can start your rehabilitation straight away. If you do not have a physiotherapist we can arrange one for you.
When the sling is removed, exercises to rehabilitate the ligaments will be started. These will improve the range of motion in your shoulder and prevent scarring as the ligaments heal. Exercises to strengthen your shoulder will gradually be added to your rehabilitation plan. Be sure to follow the treatment plan. Although it is a slow process, your commitment to physiotherapy is the most important factor in returning to all the activities you enjoy.
Download Physiotherapy protocol
When can I return to driving and work?
Return to work | Sedentary job: as tolerated |
Driving | 6-8 weeks |
Swimming | Breaststroke: 6 weeks |
Golf | 3 Months |
Lifting | Light lifting can begin at 3 weeks. Avoid lifting heavy items for 3 months. |
Contact Sport | E.g. Horse riding, football, martial arts, racket sports and rock climbing: 3 months |