Small Joint Replacements in the Hand
Osteoarthritis, also called degenerative arthritis, is a degenerative condition that commonly affects the small joints of the fingers and the base of the thumb. It can cause the joints to become swollen, stiff and painful. It often leads to joint enlargement, interfering with normal hand function and significantly affecting a person's quality of life. There are two main types of hand arthritis: primary generalised osteoarthritis and erosive osteoarthritis. They affect the hands differently.
Why have I got arthritis of my finger joints?
This condition is primarily caused by age, but more common in females and those whose job involves repetitive joint stress. As our bodies age the cartilage that lines the ends of our bones begins to weaken and can wear away. In a joint where the ends of the bones rub against each other this loss of cartilage can lead to inflammation and pain. Eventually the cartilage may completely degenerate, allowing bone to rub directly against bone. This causes further pain and difficulty with flexion. Symptoms of primary generalised osteoarthritis include pain, swelling and stiffness in the finger joints nearest the nail and base of thumb. This pain is most noticeable during and after activity, but as the condition worsens pain may be felt even during periods of limited activity. Cysts may also develop at the joints nearest the fingernails (called mucous cysts). This type of ganglion cyst may cause the overlying skin to thin or it may cause a groove to develop in the nail. Joint deformity may develop as arthritis progresses.
What are the non operative options?
Treatment options include cortisone injections, non-steroidal anti-inflammatory medications, use of a splint or brace, exercise and modification of daily activities.
Information on hydrocortisone injections. After the injection the joint should be rested for 24 hours and the sticky plaster should remain on to prevent anything from entering the puncture site. Very rarely problems can occur with steroid injections- When the local anesthetic has worn off (about 4 hours), a few patients experience some pain, this will decline over a day or two. If you are diabetic your blood sugars should be monitored for the 6 hours following the injection. Infection is very rare and is reported to occur in 1 in 15000 patients. The skin overlying the injection site can become pale and thin, this is called lipodystrophy.
Small Joint replacements of the hand
In severe cases; surgery may be needed to fuse or replace the joints.
At present there are three types of joint replacements used. Rubber (silicone), metal/plastic and pyrocarbon (a material almost as hard as diamond). Traditionally rubber joints have been used, but they provide very little stability and although excellent in patients with rheumatoid arthritis, disappointing in patients with isolated osteoarthritis of finger joints.
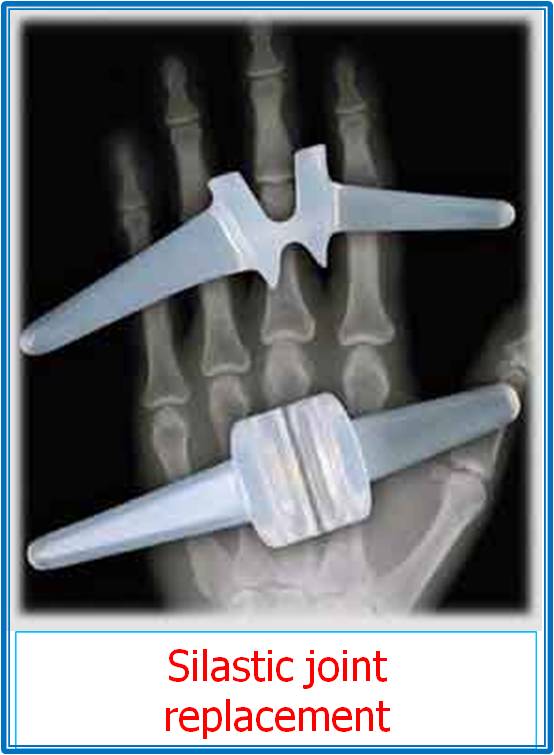
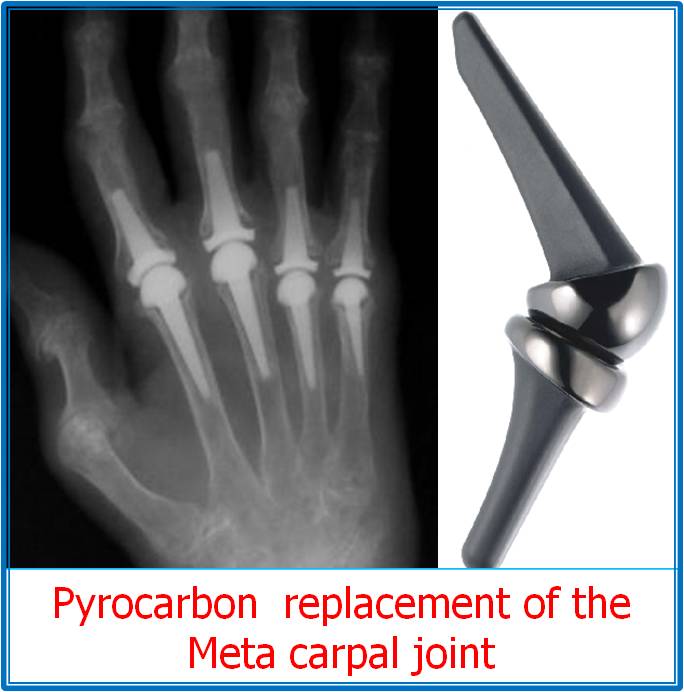
In patients with osteoarthritis who are experiencing severe pain and non operative measures have not been successful; there is a choice between 2 operations. Fusion, which results in no pain but also no movement at the finger joint, or a pyrocarbon joint replacement. Small joint replacements in the fingers provide reliable pain relief and a modest improvement in the range of movement.
Not all patients are happy with finger joint replacements and 13% require revision surgery within the first 2 years. However 80% of patients are pleased they had the operation done and those in whom the surgery was unsuccessful a fusion can be carried out (which was the original alternative).
How is the operation performed?
This is a day case operation.The choice of anesthetic will be discussed by the anesthetist, but may be a general anesthetic, where you are asleep, or a nerve block where your arm is numb, supplemented with sedation if required. During the procedure arthritic diseased bone is removed and an artificial joint is inserted.
What can I expect after surgery?
Afterwards you will have a bulky dressing, with a plaster splint. The stability of the replacement at the end of the operation will determine the speed at which you can start to regain movement and strength.
Local anaesthetic will be injected into the wound at the end of the operation. This area and the fingers will remain numb for up to six hours after surgery. Before the effect wears off, you should take painkillers which have been prescribed on a regular basis. Your hand will initially be placed in a plaster splint. Swelling causes stiffness and pain which is made worse by hanging the arm down at your side or resting it on your lap. Swelling is best prevented by keeping the hand above the level of the heart for the first 48 hours.
You will be seen within a few days by the Hand Therapist. The dressings will be removed and the wound will be checked. You will be fitted for a bespoke splint, given advice and exercises to start immediately. Hand elevation remains important to prevent swelling and stiffness of the fingers. Please remember not to walk with your hand dangling, or sit with your hand held in your lap. If the hand becomes red, hot and very swollen you must go to your GP or the Accident and Emergency Department
An appointment will be made for the following week to check your exercises. You will be given a splint to wear at night which will rest the fingers in a safe position. You will also be given a day splint to help you start bending the fingers. The surgeon will see you in the outpatient clinic around 2 weeks. Any stitches present will be removed then. Your rehabilitation will be guided by the hand therapist. At this stage it is safe to get the hand wet. The wound and the surrounding skin often become very dry and will be more comfortable if a moisturiser is applied, including on the wound itself. Initially the scar will be thickened and tender to touch. This must be massaged firmly with a moisturising cream to reduce sensitivity and swelling.
After two weeks you can usually drive a car as long as you are comfortable and have regained full finger movements. Timing of your return to work varies with your occupation and this should be discussed with your therapist.
It will take 3-6 months for the swelling to completely settle.
What are the risks?
The risks are low, but include:
- Infection - risk is low around 1%, but it occurs is a serious problem as control of infection can be difficult, due to the implant
- Pain - This usually settles over the first week and is usually moderate.
- Stiffness - Often the joint that is being replaced is very stiff. If this is the case the resultant movement after the operation will be limited. This is the most common complication in small joint replacements.
- Swelling - The finger will remain swollen for 3 to 6 months
- Nerve injury - Localised numbness around the wound may occur. It usually resolves with time.
- Dislocation - This is a risk in the short term, before the tissues tighten. The risk is low, but if it does occur, a short anaesthetic is required to relocate the joint.
- Loosening - This is the long term complication of the joint replacement and is almost inevitable. Once the joint is loose, it may become painful and swollen again. At that stage the majority of patients would have their replacement converted to a fusion. Hopefully though there have been many years of benefit!

Information for hand therapists click here.